The are 4 stages of Pneumonia symptoms of the first congestion stage include fever, chest discomfort, and a wet cough. During the hepatization stages, symptoms often get worse, and respiratory problems may occur. Usually, the illness goes away in a week or two.1. Your age, general health, and the type of germ causing the illness (bacterial vs. viral) may all affect the specific symptoms.
Table of Contents
Congestion: 4 stages of pneumonia
The first stage of pneumonia is called “congestion” because it is characterized by congestion in the lungs.
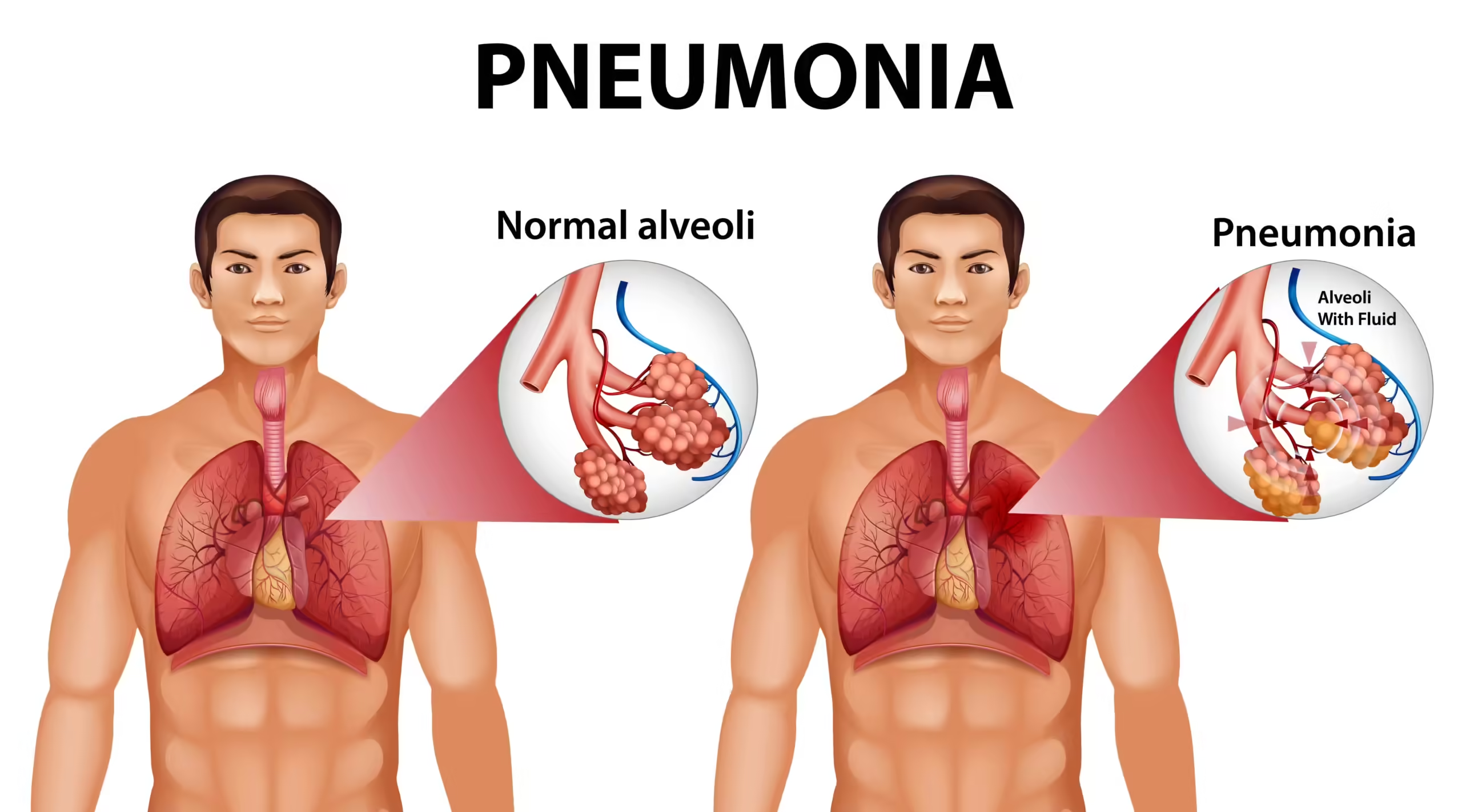
Specifically, pneumonia causes the tiny air sacs in the lungs (alveoli), as well as the tiny nearby blood vessels (capillaries), to become inflamed and congested with fluid. Most of this congestion takes place during the first 24 hours after the infection develops.2
As you breathe, an exchange of oxygen and carbon dioxide takes place between the capillaries and the alveoli. Since these are the primary structures affected by pneumonia, you will start to notice more breathing-related symptoms as the infection progresses.
Fortunately, when pneumonia is detected and promptly treated during the congestion stage, it is less likely to result in complications. However, the severity of the infection depends on several factors, including your age, overall health, and whether the infection is bacterial or viral.
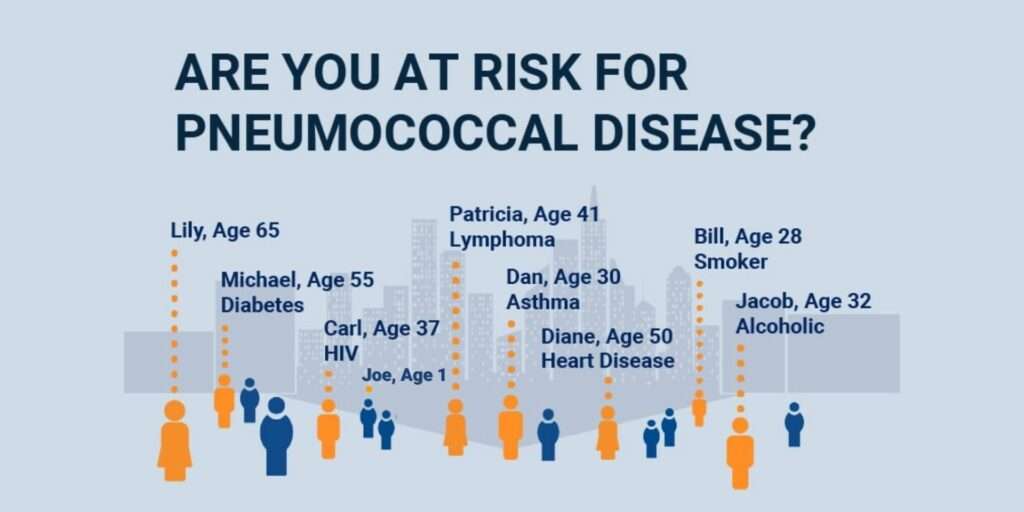
Lobar pneumonia, caused by bacterial infection, is pneumonia that affects one section (lobe) of the lungs. It’s more common than the other form of pneumonia—viral pneumonia—which is caused by viruses.

Symptoms
The congestion stage of pneumonia may start suddenly or gradually. Symptoms may be especially severe when pneumonia develops as a complication of another infection, such as influenza or COVID-19.
Symptoms in the congestion stage may include:
- Coughing, which may produce sputum that is clear, yellow, or green
- High fever and chills
- Chest pressure or heaviness
- Sharp chest pain that worsens with deep breaths (pleuritic chest pain)
- Shortness of breath
- Headache
- Loss of appetite
- Muscle aches (myalgia)
- Joint aches (arthralgia)
- Fatigue
- Nausea
- Vomiting
- Diarrhea
Some people may develop hypoxia (reduced oxygen level in the body) in the early stages of the infection. Symptoms include:
- A bluish tinge to the lips and fingers (cyanosis)
- Rapid respiratory rate (tachypnea)
- Rapid heart rate (tachycardia)
- Confusion
- Disorientation
- Shortness of breath (dyspnea)
Hemoptysis (coughing up blood) symptoms might sometimes appear even before the infection does. In any event, this may be quite concerning and needs to be checked out right away.
Adults and children frequently exhibit many of the same symptoms. Nevertheless, in certain instances, a child’s quick breathing is their sole symptom. Additionally, children may have a decrease in appetite, which can result in dehydration.
Stage 1 Symptoms in the Elderly
In older adults, typical symptoms (such as a fever or cough) may be absent, and instead, the only symptoms may be confusion or falls.
Management/Treating Symptoms of 4 stages of pneumonia
Antibiotics should be administered as soon as a diagnosis is made. Blood cultures are frequently performed as blood tests to check for the presence of germs in the blood. Treatment with antibiotics is likely to begin immediately if the infection is determined to be bacterial.
A hospital stay or admittance to an intensive care unit (ICU) may be necessary, depending on the severity. This is particularly valid for those who experience hypoxia or have trouble breathing.
In hospitals, pulse oximetry is typically used to continuously check oxygen levels through the use of a tiny finger-tip pulse oximeter device. IV (intravenous) fluids could also be required. Even at this early stage of the illness, oxygen treatment may be required if oxygen saturation is less than 92% on oximetry.5.
If early infection indicators are followed by quick antibiotic administration, the fever may go away in 48–72 hours.
Complications
The most common complication of early pneumonia (that may necessitate hospitalization) is a low oxygen level. Depending on the severity, oxygen supplementation may be needed, as well as admission to the ICU.
Red Hepatization
Pneumonia symptoms may get worse after the first twenty-four hours when red blood cells and other immune cells flood the lungs and alveoli to combat the infection.7.
Lung Association of America. The signs and diagnosis of pneumonia.
About two to three days after the infection starts, the stage known as red hepatization takes place.8
Lungs that are ordinarily pinkish-gray in appearance literally flush crimson when red blood cells fill them. Similar to a liver, low oxygen levels also make the lungs hard and dry. This liver-like look is referred to as “hepatization.”.
Symptoms
During red hepatization, symptoms are usually more severe, even if treatment has been started. These can include:
- Coughing that produces thick, yellow-green, and sometimes blood-stained phlegm
- Fever, chills, and rigors (violent shivering)
- Severe shortness of breath
- Headache
- Muscle aches
- Cyanosis, in which the lips and fingers appear blue or even blackish due to low oxygen
- Extreme fatigue
In older adults, confusion or delirium may appear even despite oxygen therapy.
The Importance of Respiratory Rate
The most useful sign as to severity at this stage is the respiratory rate (in people who do not have preexisting lung disease). A respiratory rate greater than 30 breaths per minute often means that hospitalization in intensive care is needed.
Managing/Treating Symptoms
Antibiotics are begun if a patient has not yet been examined, or they are continued (intravenously if in a hospital) during this stage of the infection. If bacterial pneumonia is the cause, blood cultures from individuals who receive an early diagnosis may reveal the specific bacterium.
Medical professionals may decide to switch up your therapy to a more suitable or targeted antibiotic based on the type of bacteria that is present. Tests known as sensitivities, which identify the antibiotic most effective against the isolated bacteria, may also be rerun to help establish the best course of treatment.
If a patient already has low oxygen levels, oxygen can be started now or continuously. Sometimes oxygen isn’t enough on its own. Using noninvasive positive pressure breathing, such as continuous positive airway pressure, or CPAP, may be a first step. Changing positions might also be beneficial since lying prone (on the stomach) increases the amount of lung surface area that is accessible for oxygen absorption.
In cases where hypoxia does not improve or if there are indications of oxygen deficiency in the body (e.g., renal malfunction), endotracheal tube implantation and mechanical breathing can be necessary.
In the event that difficulties are detected, further testing could help.
Complications
Complications may appear at any point with a diagnosis of pneumonia, but red hepatization is often when people appear most ill.
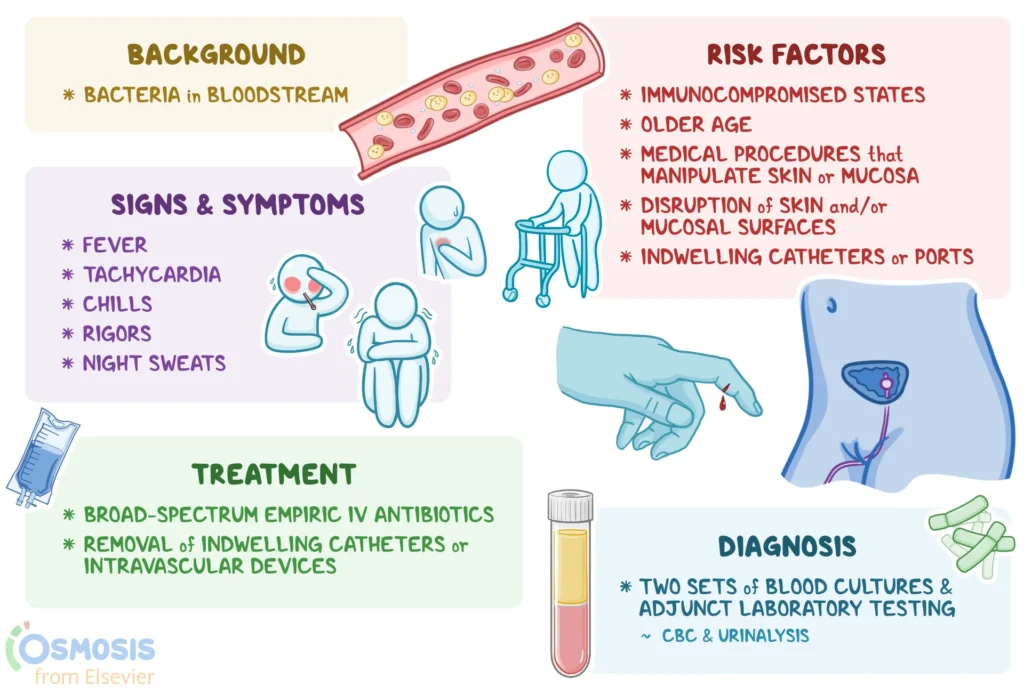
Bacteremia
Bacteria that are present in the lungs may spread in the bloodstream (bacteremia) and then travel to other regions of the body. With pneumococcal pneumonia, up to 25% to 30% of people will have bacteremia.
With bacteremia, bacteria can travel to and infect other bodily organs, including:
- The brain (meningitis)
- Heart valves (endocarditis)
- The lining of the heart (pericardium)
- Joints (septic arthritis)
- Kidneys
- Spleen
Septicemia and Sepsis
Blood poisoning, another name for septicemia, can strike at any time. While septicemia describes a condition in which bacteria are proliferating in the circulation, bacteremia describes the presence of bacteria in the bloodstream. A person suffering from septicemia would often seem quite sick, with a fast pulse and disorientation.
Sepsis, as opposed to septicemia, describes the body’s reaction to bloodstream germs. It’s crucial that the immune system responds so strongly. Sepsis is frequently deadly, even with drugs to prevent the severe inflammatory response and boost blood pressure (which is generally very low). Much research is being done on how to stop sepsis from happening.
Empyema
Pleural effusions, or accumulations of fluid between these membranes, can be caused by inflammation because lobar pneumonia frequently affects the pleura, the lining that lines the lungs. An empyema is a condition where pus accumulates and builds up between the pleural membranes.
The most frequent culprits are Staphylococcus and Streptococcus pneumoniae, which is the most prevalent cause of bacterial pneumonia. Physicians need to be on the lookout for this complication since the symptoms, which include fever, chest discomfort, coughing, and dyspnea, are similar to those of pneumonia. When imaging reveals a large pleural effusion, further workup is frequently required.
Thoracentesis is often the next procedure performed when an empyema is present. To take a sample of the fluid, a long, thin needle must be inserted through the skin and into the pleural region. After that, the sample may be examined in the lab to see whether any bacteria are present and to grow the fluid.
It could be necessary to insert a chest tube if there is a significant empyema. In order to remove the fluid, a relatively bigger tube that is left in place must be inserted into the pleural cavity and coupled to continuous suction.11
An empyema may develop in babies and children, particularly in those with Staphylococcus aureus pneumonia. Additionally, severe infections may cause a pneumothorax or collapse of the lung.
What are the Last Stages of Pneumonia Before Death?
End-stage pneumonia typically involves severe respiratory distress, requiring supplemental oxygen. Signs of oxygen deprivation, such as blue skin and an altered mental state, are usually apparent. Sepsis followed by multiple organ failure may occur and quickly lead to death.
Grey Hepatization
The third stage of pneumonia, known as grey hepatization, sets in about four to six days after the infection develops. During this stage, red blood cells begin to break up, causing the lungs to become greyish-brown or yellow in color. The lungs will become drier, too, further taking on a liver-like consistency.
Symptoms
During grey hepatization, many of the same symptoms experienced in red hepatization will persist. Breathing may become especially difficult, necessitating additional oxygen therapy or mechanical ventilation. Fits of coughing may become more severe and produce blood.6
Managing/Treating Symptoms
Antibiotics (for bacterial pneumonia) will be administered during gray hepatization. Oral antibiotics may be substituted for intravenous antibiotics in patients who are hospitalized and improving.
In the event that difficulties arise, the management of these issues may involve the use of corticosteroids in cases of an extreme immune reaction or a chest tube to control an empyema.
It is possible to start oxygen or other breathing aid for the first time, quit it altogether, or continue using it.
Careful monitoring and management of additional consequences, such as renal failure, dehydration, and other issues, will be necessary for hospitalized patients.
Complications
Complications noted in the earlier stages of pneumonia may not occur until grey hepatization for some people, especially those who have not received treatment.
For those who have a severe infection, a lung abscess may form.
In addition to symptoms associated with pneumonia—such as fever and cough—other symptoms of a lung abscess can include:
- An increase in sputum that can become foul-smelling
- Worsening of cough and fever, if they had been improving
- Night sweats (drenching sweats that require getting up and changing pajamas) can occur
- Weight loss in those who develop an abscess sometime after their pneumonia occurred
- Coughing up blood (quite common)
An abscess itself can also lead to further complications, such as:
- An empyema (if not already present)
- A bronchopleural fistula (an abnormal passageway between the bronchi and the pleural cavity)
- Bleeding into the lungs
Treatment begins with broad-spectrum antibiotics (a lung abscess will usually require a change in antibiotics being used). If this is ineffective, the abscess may need to be drained (often with a long, narrow needle inserted through the skin).
In some cases, surgical removal of the abscess will be needed. Follow-up is also very important, as underlying lung cancer has been found in one to two out of 10 lung abscesses.
What Are the Worst Days of Pneumonia?
Pneumonia can be unpredictable and complications may occur at any time. In most cases, pneumonia peaks during the hepatization stages, in which the risk of hypoxia (low oxygen) and severe complications is particularly high. Research shows the mortality rate for people with pneumonia placed in the ICU (intensive care unit) is approximately 15% to 50%
Resolution
The final stage of pneumonia, known as resolution, depends on how quickly treatment is started. Ordinarily, resolution of the infection occurs around eight days after the start of the infection.
In children, it can take two to three weeks for mild pneumonia to resolve, or up to eight weeks for pneumonia that is severe.16
This recovery stage includes:
- Resolution of the infection
- Restoration of the normal airways and alveoli
At this point in the infection, the immune system works to repair the damage to the lungs. This includes the release of enzymes that break down damaged tissue so that it can be reabsorbed. An influx of cells called macrophages will travel through the lungs and “eat” (phagocytize) debris and white cells containing bacteria.
Leftover debris in the lungs that can’t be eliminated in this way is usually coughed up
Symptoms
Since debris in the lungs that can’t otherwise be removed is coughed up, a cough productive of sputum is very common at this stage. Knowing that the body is continuing to repair damage that was done during the infection can help explain the fatigue often present (and why rest is still important).
If untreated (and in some cases even with treatment), respiratory symptoms may worsen, When treatment is started early, however, and no serious complications have occurred, symptoms usually improve significantly at this point in time (except for the cough).
If scar tissue develops in the pleura (pleural adhesions), pain with a deep breath may occur and may last for quite some time.
Managing/Treating Symptoms
Typically, antibiotics are used for a minimum of 10 days. Antibiotics may be switched to oral pills if they were previously administered intravenously. Many hospitalized patients may be released from care (if they haven’t already).
It could be necessary to start oxygen or mechanical breathing at this point for people whose condition doesn’t improve. Long-term oxygen treatment may be required in some situations. Conversely, patients whose health is improving and they were receiving supplementary oxygen may begin to wean themselves off of oxygen therapy.
Complications
Complications discussed at other stages may occur later in the infection, especially lung abscesses.
The repair process may result in scar tissue in the lung linings (pleural adhesions) that may affect care in the future. For example, it could cause problems with pleural effusions or lung cancer surgery down the road.
Roughly 10% to 15% of people will have a recurrent episode of pneumonia within two years of the infection.6
Jameson JL, Fauci AS, Kasper KL, et al (Eds.). Harrison’s Principles of Internal Medicine. McGraw-Hill Education.
For some people, lung damage may persist, requiring long-term oxygen supplementation. Severe pneumonia may also worsen underlying chronic obstructive pulmonary disease (COPD).
How Can You Tell if Pneumonia Is Getting Better or Worse?
Most people with pneumonia start to feel better within a few days of starting treatment with antibiotics. It is a good sign that you are recovering if your temperature returns to normal within seven days. You should be coughing less, breathing better, and feeling less chest pressure as time goes on. Contact your healthcare provider if this isn’t the case.
Summary
There are four phases of pneumonia, which might have bacterial or viral causes: congestion, red, gray, and resolution hepatization. The way the infection affects the lungs is indicated by the nomenclature of each stage. Congestion frequently presents with flu-like symptoms, but developing respiratory problems and an increased risk of complications are hallmarks of the hepatization phases.
During the resolution stage, the body makes a lot of effort to heal the lungs, although long-term lung damage could still exist. At different phases of the infection, many patients with pneumonia need extra oxygen; for some, oxygen treatment will be necessary for an extended period of time.